Breast cancer is a serious health issue that affects many women. Regular mammograms can help find breast cancer early, making it easier to treat. There are different guidelines about when and how often women should get mammograms. These guidelines can be confusing, but they are important to understand.
Key Takeaways
- Women aged 40 to 74 should get a mammogram every 2 years.
- Digital and 3D mammography are both effective for screening.
- It's important that everyone gets equal follow-up care after an abnormal mammogram.
- There isn't enough evidence to say if women over 75 should get mammograms.
- Doctors should help women decide about extra screening if they have dense breasts.
Understanding Mammogram Guidelines
Importance of Early Detection
Early detection of breast cancer can save lives. Mammograms can find changes in the breast years before any physical symptoms appear. This early detection often means less aggressive treatments and a higher chance of being cured.
Differences in Guidelines by Organizations
Different health organizations have varying recommendations for mammogram screenings. For example:
- The American Cancer Society suggests women aged 45 to 54 get yearly mammograms, while those 55 and older can switch to every two years.
- The U.S. Preventive Services Task Force recommends biennial screenings for women aged 50 to 74.
These differences arise from how each organization weighs the benefits and harms of screening.
Impact of Updated Guidelines
Updated guidelines can influence when and how often women get screened. They aim to balance the benefits of early cancer detection with the risks of overdiagnosis and false positives. It's crucial for women to discuss these guidelines with their healthcare providers to make informed decisions.
Understanding the guidelines helps women make better choices about their health. Always talk to your doctor to see what’s best for you.
Screening Recommendations for Different Age Groups
Women Aged 40 to 49
For women in their 40s, the guidelines vary. Some organizations recommend starting annual mammograms at age 40, while others suggest beginning at age 45. The decision should be made through shared decision-making, considering the benefits and potential harms.
Women Aged 50 to 74
Women aged 50 to 74 are generally advised to have mammograms every 1 to 2 years. This age group benefits the most from regular screening, as the risk of breast cancer increases with age. Biennial screening is often recommended to balance the benefits and harms.
Women Aged 75 and Older
For women 75 and older, the recommendations are less clear. Some guidelines suggest continuing mammograms if the woman is in good health and has a life expectancy of 10 years or more. However, there is limited evidence on the benefits of screening in this age group. The decision should be individualized, taking into account the woman's overall health and preferences.
Types of Mammographic Screening
Digital Mammography
Digital mammography uses low-dose X-rays to create images of the breast. This method is widely used and has been proven effective in detecting breast cancer early. It offers clear images that can be easily stored and shared with other healthcare providers. However, it may not be as effective for women with dense breast tissue.
3D Mammography
Also known as digital breast tomosynthesis, 3D mammography takes multiple images of the breast from different angles. This creates a three-dimensional picture, making it easier to spot abnormalities. Studies suggest that 3D mammography reduces the need for follow-up tests and is particularly useful for women with dense breasts. However, it can be more expensive and may not be covered by all insurance plans.
Supplemental Screening Methods
In addition to standard mammograms, other screening methods can be used to detect breast cancer:
- Ultrasound: Often used for women with dense breast tissue, ultrasound can help identify abnormalities that a mammogram might miss.
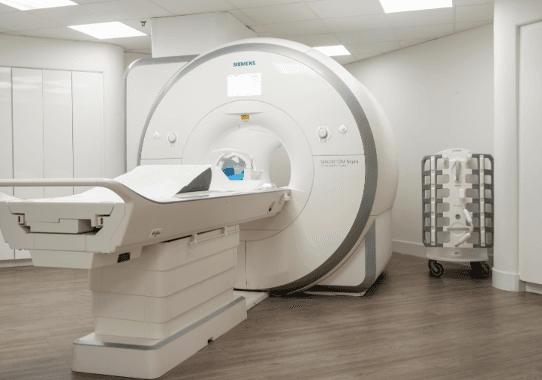
- MRI: Magnetic Resonance Imaging (MRI) is another option, especially for high-risk women. It provides detailed images but is more costly and time-consuming.
- Clinical Breast Exams (CBE) and Breast Self-Exams (BSE): While not as effective as mammograms, these methods can still play a role in early detection. Women should be familiar with how their breasts normally look and feel and report any changes to their healthcare provider.
It's important to discuss with your healthcare provider which screening method is best for you, considering your individual risk factors and the pros and cons of each method.
Shared Decision-Making in Breast Cancer Screening
Discussing Benefits and Harms
Shared decision-making is a process where patients and doctors work together to make choices about treatments. This is especially important for breast cancer screening because it involves weighing the benefits, like early detection, against the harms, such as false positives and overdiagnosis. Doctors provide the medical facts, while patients share their personal values and concerns.
Incorporating Patient Values
Incorporating patient values means understanding what is important to the patient. This can include their experiences, fears, and priorities. Doctors can use tools like online videos, handouts, or face-to-face talks to help patients understand their options. This ensures that the patient's voice is heard in the decision-making process.
Role of Healthcare Providers
Healthcare providers play a crucial role in shared decision-making. They must present information clearly and help patients understand the potential outcomes of different screening options. Providers should also respect the patient's preferences and support them in making informed choices.
Shared decision-making helps ensure that breast cancer screening decisions align with the patient's values and lifestyle.
Addressing Disparities in Breast Cancer Screening
Equitable Follow-Up Evaluation
Disparities in follow-up after screening and treatment have been observed for Asian, Black, and Hispanic women. Ensuring timely and effective follow-up care is crucial to reducing mortality rates among these groups. Improvements in access to healthcare, removal of financial barriers, and use of support services can help achieve this goal.
Access to Additional Testing
Access to additional testing, such as genetic counseling and advanced imaging, is often limited for minority groups. This lack of access can lead to delayed diagnoses and poorer outcomes. Efforts should be made to provide equitable access to these essential services.
Ensuring Effective Treatment
Black women are more likely to discontinue adjuvant endocrine therapy due to greater physical and psychological symptom burdens. Providing support to manage these symptoms can improve adherence to treatment. Additionally, addressing structural racism and improving healthcare delivery can ensure that all women receive high-quality treatment.
Benefits and Limitations of Mammographic Screening
Reduction in Mortality
Mammographic screening has been shown to reduce the number of deaths from breast cancer. Early detection through regular mammograms can catch cancer at a more treatable stage. This is especially true for women aged 40 to 74, where biennial screening has a moderate benefit in lowering mortality rates.
Potential Harms and False Positives
Screening mammograms can sometimes lead to false-positive results. This means that the test suggests cancer is present when it is not. False positives can cause anxiety and lead to additional tests, such as biopsies, which may be unnecessary. The likelihood of false positives is higher with annual screenings compared to biennial ones.
Overdiagnosis Concerns
Overdiagnosis is another limitation of mammographic screening. This occurs when the screening detects a cancer that would not have caused any problems during the person's lifetime. Overdiagnosis can lead to overtreatment, including surgeries, radiation, and chemotherapy, which have their own risks and side effects.
While mammographic screening has clear benefits, it is important to weigh these against the potential harms. Discussing these factors with a healthcare provider can help in making an informed decision.
Clinical Considerations and Recommendations

Assessing Breast Cancer Risk
Healthcare providers should regularly evaluate a woman's risk of breast cancer by reviewing her medical history. This includes looking at reproductive factors, past biopsies, radiation exposure, and family history of cancers. Women with a higher risk based on initial assessments should undergo further evaluation. Tools like the Gail model or the BRCAPRO can help in this assessment.
Frequency of Screening
For women at average risk, screening mammography should start at age 40. The frequency can be every 1 or 2 years, depending on a shared decision-making process that considers the benefits and harms. Women should continue screening until at least age 75.
Guidelines for High-Risk Women
Women identified as high-risk may need more frequent screenings and additional tests like MRI. They might also benefit from genetic counseling and risk-reduction strategies. Regular clinical breast exams and enhanced screening methods are recommended for these women.
It's crucial to tailor breast cancer screening to each woman's risk level and personal preferences, ensuring the best possible outcomes.
Conclusion
In conclusion, regular mammograms are a key tool in the early detection and treatment of breast cancer. By following the recommended guidelines, women can significantly increase their chances of catching cancer early when it is most treatable. It's important for women to start discussing mammogram options with their healthcare providers by age 40 and to continue these discussions as they age. While there are different recommendations based on age and risk factors, the consensus is clear: regular screening saves lives. Women should feel empowered to make informed decisions about their health and take advantage of the screening options available to them.
Frequently Asked Questions
At what age should women start getting mammograms?
Women should start getting mammograms at age 40. For those aged 45 to 54, yearly mammograms are recommended. Women 55 and older can switch to every other year or continue yearly screenings.
What types of mammograms are available?
There are two main types of mammograms: digital mammography and 3D mammography (also known as digital breast tomosynthesis). Both are effective for breast cancer screening.
How often should women get mammograms?
Women aged 40 to 74 should get a mammogram every 1 to 2 years. The frequency can be decided based on a discussion with their healthcare provider about the benefits and risks.
Are mammograms necessary for women over 75?
There is not enough evidence to recommend for or against mammograms for women over 75. The decision should be made by the woman and her healthcare provider, considering her overall health.
What should women with dense breasts do about screening?
Women with dense breasts should discuss with their healthcare provider whether they need additional screening methods like breast ultrasound or MRI, in addition to regular mammograms.
What are the benefits and risks of mammograms?
Mammograms can help detect breast cancer early, increasing the chances of successful treatment. However, they can also lead to false positives and overdiagnosis, which may cause unnecessary stress and treatment.