Ovarian cancer is a serious illness that affects thousands of women each year. Detecting it early can make a big difference in treatment success. This article will help you understand the early symptoms, risk factors, diagnostic methods, and treatment options for ovarian cancer. We will also discuss how to live with the disease and steps you can take to prevent it.
Key Takeaways
- Early signs of ovarian cancer can be subtle, including bloating and changes in eating habits.
- Family history and genetic mutations increase the risk of developing ovarian cancer.
- Regular pelvic exams and imaging tests help in diagnosing ovarian cancer.
- Treatment options include surgery, chemotherapy, and targeted therapies.
- Emotional and psychological support is crucial for those living with ovarian cancer.
Recognizing Early Symptoms of Ovarian Cancer
Abdominal Bloating and Pain
One of the earliest signs of ovarian cancer is persistent abdominal bloating. This bloating can be so severe that it makes the abdomen look swollen. Along with bloating, women may experience abdominal or pelvic pain that doesn't go away.
Changes in Eating Habits
Women with ovarian cancer often notice changes in their eating habits. They may feel full quickly after starting a meal or lose their appetite altogether. This can lead to unintentional weight loss.
Urinary Symptoms
Frequent urination or an urgent need to urinate can also be early signs of ovarian cancer. These symptoms occur because the growing tumor puts pressure on the bladder. If you notice these symptoms and they persist, it's important to consult a healthcare provider.
Early detection of ovarian cancer can significantly improve treatment outcomes. If you experience any of these symptoms consistently, seek medical advice promptly.
Risk Factors and Genetic Predispositions
Family History and Genetic Mutations
A family history of ovarian cancer can significantly increase your risk. Genetic mutations, especially in the BRCA1 and BRCA2 genes, are major risk factors. These genes normally help prevent cancer by repairing DNA, but mutations can lead to cancer. If one of your parents has a BRCA mutation, you have a 50% chance of inheriting it.
Age and Menstrual History
Age is another important factor. Most ovarian cancers are diagnosed in women aged 55 to 64. Early menstruation (before age 12) or late menopause (after age 52) can also increase the risk. The more menstrual cycles a woman has, the higher her risk.
Lifestyle and Environmental Factors
Certain lifestyle choices and environmental factors can also contribute to the risk of ovarian cancer. These include:
- Being overweight or obese
- Using hormone replacement therapy (HRT) for menopause symptoms
- Having endometriosis, a condition where tissue similar to the lining inside the uterus grows outside it
- Smoking, which slightly increases the risk
- Ethnicity, with higher risks in Eastern European or Ashkenazi Jewish backgrounds
Understanding these risk factors can help in making informed decisions about your health. Regular check-ups and discussions with your doctor are crucial for early detection and prevention.
Diagnostic Methods for Ovarian Cancer
Pelvic Examinations
Doctors often start with a pelvic exam to check for any unusual growths or changes in the ovaries and uterus. However, small tumors can be hard to detect this way. As the tumor grows, it may press against other organs, making it easier to feel during an exam.
Imaging Techniques
Several imaging tests can help identify ovarian cancer:
- Transvaginal Ultrasound (TVUS): Uses sound waves to create images of the ovaries and can detect tumors, but it can't tell if they are cancerous.
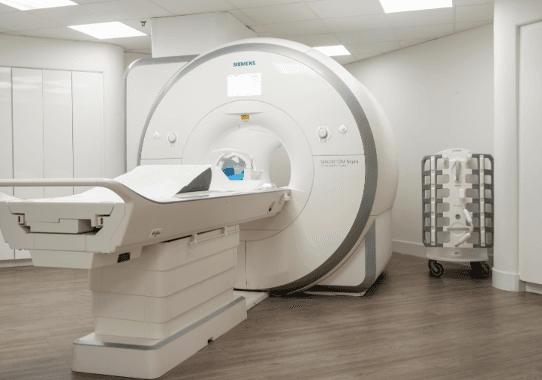
- CT Scan: Provides detailed images of the abdomen and pelvis. If you're allergic to dye, a pelvic MRI may be used instead.
- MRI: Offers detailed images and is an alternative for those who can't undergo a CT scan.
- PET Scan: Uses a special dye with radioactive tracers to show how well organs and tissues are functioning.
Blood Tests and Biomarkers
Blood tests can look for markers that indicate cancer. The CA-125 test measures a protein that is often higher in women with ovarian cancer. However, high levels can also be due to other conditions like menstruation or fibroids. Because of this, blood tests are usually combined with other diagnostic methods.
A biopsy is the only way to confirm if a tumor is cancerous. This involves taking a small tissue sample from the ovary and examining it under a microscope.
Treatment Options for Ovarian Cancer
Surgical Interventions
Surgery is often the first step in treating ovarian cancer. The main goal is to remove as much of the tumor as possible. This may involve a hysterectomy, which is the removal of the uterus, and often includes removing both ovaries and fallopian tubes, nearby lymph nodes, and other affected tissues. In some cases, only one ovary may be removed to preserve fertility.
Chemotherapy and Radiation
Chemotherapy uses drugs to kill cancer cells and is usually given after surgery to target any remaining cancer cells. It can be administered intravenously or orally. Radiation therapy, though less common, uses high-energy particles or X-rays to destroy cancer cells and is typically used when the cancer has spread beyond the ovaries.
Targeted and Hormonal Therapies
Targeted therapy focuses on attacking cancer cells while minimizing damage to normal cells. Newer targeted therapies include PARP inhibitors like olaparib (Lynparza), niraparib (Zejula), and rucaparib (Rubraca). These drugs block an enzyme that helps repair DNA in cells, making it harder for cancer cells to survive. Hormonal therapy blocks hormones that fuel certain types of ovarian cancer, slowing or stopping their growth.
It's important to discuss all treatment options with your healthcare provider to choose the best plan tailored to your needs.
Living with Ovarian Cancer
Managing Side Effects
Living with ovarian cancer often means dealing with side effects from treatments. These can include fatigue, nausea, and hair loss. It's important to communicate with your healthcare provider about any side effects you experience, as they can offer solutions to help manage them. Sometimes, simple lifestyle changes can make a big difference.
Emotional and Psychological Support
A diagnosis of ovarian cancer can be emotionally challenging. Feelings of sadness, frustration, and anxiety are common. Support groups, either local or online, can provide a sense of community and understanding. Talking to a mental health professional can also be beneficial.
Follow-Up Care and Monitoring
After treatment, regular follow-up appointments are crucial. During these visits, your healthcare provider will check for any signs of cancer returning and address any new symptoms. Staying vigilant and reporting any unusual changes in your body can help catch potential issues early. Routine imaging tests, like CT scans, may also be part of your follow-up care.
Preventive Measures and Early Detection

Regular Health Screenings
Regular health screenings are crucial for early detection of ovarian cancer. Pelvic exams can help identify abnormalities in the ovaries and uterus, although they may not always detect early-stage ovarian cancer. It's important to discuss the need for these exams with your doctor.
Genetic Counseling and Testing
Genetic counseling and testing can identify individuals at higher risk for ovarian cancer. If you have a family history of ovarian or related cancers, genetic testing for mutations like BRCA1 and BRCA2 can be beneficial. This information can guide you and your healthcare provider in making informed decisions about your health.
Lifestyle Modifications
Certain lifestyle changes can help reduce the risk of ovarian cancer:
- Maintain a healthy weight: Obesity has been linked to an increased risk of various cancers, including ovarian cancer.
- Healthy diet: A diet rich in fruits, vegetables, and whole grains can support overall health and potentially lower cancer risk.
- Avoid tobacco: Smoking is a known risk factor for many cancers.
- Regular exercise: Physical activity can help maintain a healthy weight and reduce cancer risk.
Taking proactive steps in your health can make a significant difference in early detection and prevention of ovarian cancer. Regular check-ups, understanding your genetic risk, and making healthy lifestyle choices are key components in this fight.
Conclusion
Ovarian cancer is a serious disease, but knowing the early signs can make a big difference. Symptoms like bloating, belly pain, and feeling full quickly should not be ignored. Early detection is key because it can lead to better treatment outcomes. Regular check-ups and talking to your doctor about any unusual changes can help catch the disease early. Remember, being aware and proactive about your health is the best way to fight ovarian cancer.
Frequently Asked Questions
What are the early signs of ovarian cancer?
Early signs of ovarian cancer can be subtle and easy to miss. Common symptoms include abdominal bloating, pain, feeling full quickly when eating, and frequent urination.
How is ovarian cancer diagnosed?
Doctors use several methods to diagnose ovarian cancer, including pelvic exams, imaging tests like ultrasounds or CT scans, and blood tests that look for specific markers.
Can ovarian cancer be detected early?
Early detection of ovarian cancer is challenging because symptoms are often vague. Regular health check-ups and being aware of your body can help in catching it early.
What are the treatment options for ovarian cancer?
Treatment options include surgery to remove the tumor, chemotherapy, radiation, and targeted therapies that focus on specific aspects of the cancer cells.
Who is at risk for ovarian cancer?
Risk factors include a family history of ovarian cancer, genetic mutations like BRCA1 and BRCA2, age, and certain lifestyle factors such as smoking or being overweight.
How can I support a loved one with ovarian cancer?
Supporting a loved one with ovarian cancer involves being there for emotional support, helping with daily tasks, and encouraging them to follow their treatment plan and attend medical appointments.