Antibiotics are powerful medicines that fight bacterial infections, saving countless lives. However, they don't just target harmful bacteria; they also disrupt the beneficial bacteria in our gut. This imbalance can lead to various health issues. Understanding how antibiotics affect your gut and learning ways to rebuild it is crucial for maintaining overall health.
Key Takeaways
- Antibiotics can disrupt the balance of good and bad bacteria in your gut, leading to health problems.
- The gut microbiome usually starts to recover within a few weeks after finishing antibiotics, but it may take months to fully restore.
- Probiotics and prebiotic foods can help support the growth of beneficial bacteria during and after antibiotic treatment.
- A balanced diet rich in fiber and fermented foods can aid in replenishing your gut flora.
- Managing stress and getting enough sleep are also important for gut health recovery.
Understanding the Impact of Antibiotics on Gut Health
How Antibiotics Disrupt Gut Microbiota
Antibiotics are designed to kill harmful bacteria causing infections, but they don't discriminate between good and bad bacteria. This means they can also destroy beneficial bacteria in your gut. When this happens, the diversity and richness of your gut microbiome decrease significantly. Some species may even disappear for a short or long period. The extent of this disruption depends on factors like the type of antibiotic used and the individual's gut microbiome resilience.
Short-term and Long-term Effects
In the short term, antibiotics can lead to a drop in beneficial bacteria and an overgrowth of harmful bacteria like Streptococcus and Lactobacillus. Over time, the gut microbiome may not return to its original state, even months after stopping antibiotics. This phenomenon is sometimes referred to as "antibiotic scarring." Long-term effects can include an increase in antibiotic-resistant genes, making future infections harder to treat.
Factors Influencing Gut Microbiome Resilience
Several factors influence how well your gut microbiome can bounce back after antibiotic use:
- Type of Antibiotic: Broad-spectrum antibiotics affect a wider range of bacteria compared to narrow-spectrum antibiotics.
- Individual Differences: Some people naturally have a more resilient gut microbiome.
- Age: Early exposure to antibiotics can have lasting effects on gut health.
- Previous Antibiotic Use: Frequent use of antibiotics can make the gut microbiome less resilient over time.
It's crucial to think twice before using antibiotics and consider whether they are truly necessary. Overuse can lead to long-lasting changes in your gut health.
The Phases of Gut Microbiome Recovery Post-Antibiotics
Initial Disruption and Loss of Diversity
When you take antibiotics, they don't just target the bad bacteria causing your infection. They also wipe out many of the good bacteria in your gut. This leads to a significant drop in the variety and number of gut microbes. Some beneficial species may even disappear for a while, making your gut less diverse and more vulnerable.
Rise of Pathogenic Bacteria
With fewer good bacteria around, harmful bacteria can start to take over. This imbalance can lead to issues like antibiotic-associated diarrhea. Drug-resistant bacteria, in particular, can grow unchecked, increasing the number of antibiotic resistance genes in your gut.
Gradual Recolonization of Beneficial Bacteria
After finishing your antibiotics, your gut will slowly start to recover. Beneficial bacteria will begin to repopulate, but this process can take time. For most people, it takes about one to two months for the gut microbiome to return to its original state. However, some may take longer, and a few might not fully recover their previous gut diversity.
Strategies to Support Gut Health During and After Antibiotic Use
The Role of Probiotics
Taking probiotics during and after antibiotic treatment can be beneficial. Probiotics are live microorganisms that help restore the balance of gut bacteria. They can be found in supplements and fermented foods like yogurt and kefir. It's recommended to take probiotics at least 2 hours after your antibiotic dose to ensure they are effective.
Incorporating Prebiotic Foods
Prebiotics are types of fiber that feed the good bacteria in your gut. Foods rich in prebiotics include whole grains, bananas, onions, garlic, and apples. Including these in your diet can help promote the growth of beneficial bacteria.
Importance of a Balanced Diet
A balanced diet is crucial for maintaining gut health. Focus on eating a variety of fruits, vegetables, lean proteins, and whole grains. Avoid processed foods, excess sugar, and unhealthy fats, as they can harm your gut microbiome.
Supporting your gut health during and after antibiotic use is essential for overall well-being. By incorporating probiotics, prebiotic foods, and maintaining a balanced diet, you can help your gut recover and thrive.
Dietary Recommendations for Rebuilding Gut Flora
High-Fiber Foods and Their Benefits
High-fiber foods are essential for promoting the growth of beneficial bacteria in the gut. These foods act as prebiotics, which means they feed the good bacteria. Some excellent high-fiber foods include:
- Whole grains like oats and barley
- Lentils and beans
- Fruits such as apples and bananas
- Vegetables like broccoli and artichokes
- Nuts and seeds
Fermented Foods to Include
Fermented foods are rich in probiotics, which are live beneficial bacteria. Including these in your diet can help restore your gut flora. Some fermented foods to consider are:
- Yogurt
- Sauerkraut
- Kimchi
- Kombucha
- Cheese
Foods to Avoid for Optimal Gut Health
Certain foods can hinder the recovery of your gut flora. It's best to avoid:
- Sugary snacks and beverages
- Processed foods
- Red meat
- Artificial sweeteners
A balanced diet rich in fiber and fermented foods can significantly aid in rebuilding your gut flora after antibiotic use.
Lifestyle Factors That Influence Gut Recovery
Managing Stress for Gut Health
Stress can have a significant impact on your gut health. High stress levels can disrupt the balance of bacteria in your gut, leading to issues like inflammation and digestive problems. To manage stress, consider activities like yoga, meditation, or even simple breathing exercises. Reducing stress not only helps your gut but also improves your overall well-being.
The Gut-Brain Connection
The gut-brain connection is a two-way street. Your gut health can affect your mood and vice versa. This connection is often referred to as the gut-brain axis. When your gut is healthy, it can produce neurotransmitters like serotonin, which help regulate your mood. On the flip side, poor gut health can lead to mood swings and even depression. Keeping both your gut and brain healthy is crucial for overall wellness.
The Role of Sleep in Gut Health
Getting enough sleep is essential for gut health. Lack of sleep can slow down your metabolism and cause issues like constipation and inflammation. Aim for 7-9 hours of quality sleep each night. Good sleep hygiene practices, such as maintaining a regular sleep schedule and avoiding screens before bedtime, can make a big difference.
Remember, a healthy lifestyle is key to gut recovery. Manage your stress, pay attention to the gut-brain connection, and ensure you get enough sleep. Your gut will thank you.
Monitoring and Tracking Gut Health Post-Antibiotics
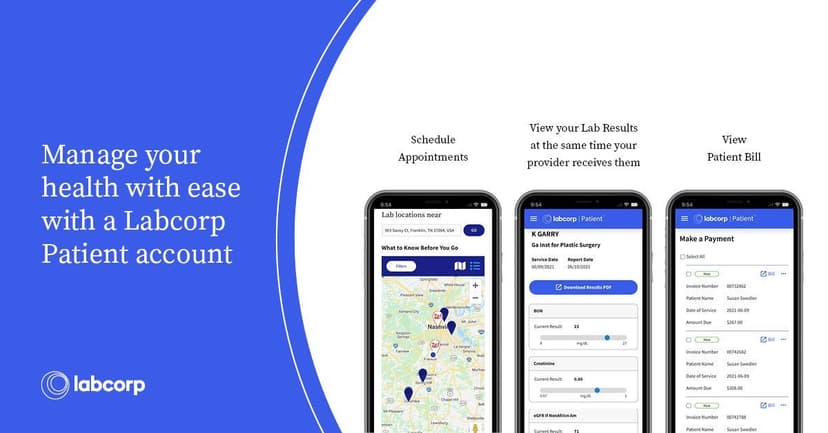
Using Gut Microbiome Tests
After finishing a course of antibiotics, it's important to monitor your gut health. Gut microbiome tests can provide valuable insights into how your gut bacteria are recovering. These tests can:
- Detect antibiotic-resistant bacteria
- Show if you still need probiotic support
- Reveal any antibiotic signatures linked to health risks
Identifying Signs of Gut Imbalance
Pay attention to your body. Signs that your gut might be out of balance include:
- Persistent digestive issues like bloating or diarrhea
- Unexplained fatigue
- Frequent infections
When to Seek Professional Help
If you notice ongoing issues with your gut health, it might be time to consult a healthcare professional. They can offer personalized advice and treatment options to help restore your gut flora.
Monitoring your gut health after antibiotics is crucial for long-term well-being. Trust your body and take proactive steps to support your recovery.
Common Myths and Misconceptions About Gut Health and Antibiotics
Myth: All Probiotics Are the Same
Not all probiotics are created equal. Different strains of probiotics have different effects on the gut. It's important to choose the right strain for your specific needs. For example, some probiotics are better for digestive health, while others may boost the immune system.
Misconception: Gut Health Recovers Instantly
Many people believe that their gut health will bounce back immediately after finishing a course of antibiotics. However, this is not the case. Recovery can take time, and the duration varies from person to person. Factors like diet, lifestyle, and the initial state of your gut microbiome play significant roles in how quickly you can restore your gut health.
Myth: Antibiotics Only Affect Gut Bacteria
Antibiotics are designed to kill harmful bacteria, but they don't discriminate. They can also kill beneficial bacteria in your gut, leading to an imbalance. This imbalance can cause various issues, such as digestive problems and weakened immunity. It's crucial to take steps to rebuild your gut flora after antibiotic use, such as consuming probiotics and prebiotics, eating a balanced diet, and managing stress.
Remember, while antibiotics are sometimes necessary, they can have a lasting impact on your gut health. Taking proactive steps to support your gut can make a significant difference in your overall well-being.
Conclusion
Antibiotics are essential for fighting infections, but they can also disrupt the balance of good and bad bacteria in your gut. This imbalance can lead to various health issues, but the good news is that your gut can recover. By eating a diet rich in fiber, fermented foods, and probiotics, you can help restore your gut's healthy bacteria. It's also important to manage stress and get enough sleep, as these factors can impact your gut health. While it may take some time, with the right steps, you can rebuild your gut and support your overall well-being.
Frequently Asked Questions
How do antibiotics affect gut health?
Antibiotics kill both harmful and beneficial bacteria in your gut, disrupting the balance and potentially leading to digestive issues and other health problems.
Can the gut microbiome recover after antibiotic use?
Yes, the gut microbiome can recover, but it may take weeks to months. Some beneficial bacteria might not return even after six months.
What are some signs of an imbalanced gut after antibiotics?
Signs of an imbalanced gut include digestive issues like diarrhea or constipation, bloating, and a weakened immune system.
How can probiotics help during and after antibiotics?
Probiotics can help restore the balance of good bacteria in your gut, reducing the negative effects of antibiotics and promoting faster recovery.
What foods support gut health after antibiotics?
Foods high in fiber, fermented foods like yogurt and sauerkraut, and prebiotic foods like bananas and garlic can support gut health.
When should I seek professional help for gut health issues?
If you experience severe or persistent digestive problems, it's important to consult a healthcare professional for proper diagnosis and treatment.