Endometriosis is a condition where tissue similar to the lining inside the uterus starts to grow outside of it. This can cause a lot of pain, especially during periods, and can also lead to fertility issues. While there's no cure, there are many ways to manage the symptoms and improve quality of life. Knowing more about endometriosis can help those affected make better decisions about their health.
Key Takeaways
- Endometriosis causes tissue similar to the uterine lining to grow outside the uterus, leading to pain and fertility issues.
- Common symptoms include severe menstrual cramps, chronic pelvic pain, and pain during intercourse.
- Diagnosis often involves a pelvic exam, imaging tests, and sometimes a laparoscopy.
- Treatment options include pain relief medications, hormonal therapies, and in some cases, surgery.
- Living with endometriosis can be challenging, but support groups and lifestyle changes can help manage the condition.
Understanding Endometriosis
What is Endometriosis?
Endometriosis is a condition where tissue similar to the lining inside the uterus starts to grow outside the uterus. This tissue can be found on the ovaries, fallopian tubes, and other areas within the pelvis. During menstrual cycles, this tissue behaves like normal uterine lining, thickening and breaking down, but it has no way to exit the body. This can lead to pain and other complications.
Causes and Risk Factors
The exact cause of endometriosis is not known, but several factors may increase the risk:
- Genetics: If a close family member has endometriosis, you might be more likely to develop it.
- Menstrual Cycle Factors: Short menstrual cycles, heavy periods, or periods lasting longer than seven days can increase risk.
- Hormones: Estrogen seems to promote endometriosis.
- Immune System Issues: Problems with the immune system may make the body less able to recognize and destroy endometrial-like tissue growing outside the uterus.
How Endometriosis Affects the Body
Endometriosis can cause a range of symptoms and complications, including:
- Pain: This is the most common symptom, often occurring in the pelvic area, especially during menstruation.
- Scar Tissue: The condition can cause scar tissue and adhesions, which can bind organs together.
- Cysts: Sometimes, endometriosis leads to the formation of cysts on the ovaries, known as endometriomas.
- Fertility Issues: Endometriosis can make it harder to get pregnant.
Living with endometriosis can be challenging, but understanding the condition is the first step toward managing it effectively.
Recognizing the Symptoms of Endometriosis
Common Symptoms
Endometriosis can present a variety of symptoms, which can differ in severity from person to person. Common symptoms include:
- Painful periods (dysmenorrhea): Pelvic pain and cramping may start before and extend several days into your period. You might also experience lower back and abdominal pain.
- Pain during or after sex: This is a frequent symptom of endometriosis.
- Pain with bowel movements or urination: These symptoms are more likely to occur during your period.
- Excessive bleeding: You may have heavy menstrual periods or bleeding between periods.
- Infertility: Endometriosis is sometimes first diagnosed in those seeking treatment for infertility.
- Other symptoms: Fatigue, diarrhea, constipation, bloating, and nausea, especially during menstrual periods.
Less Common Symptoms
While the above symptoms are more typical, some individuals may experience less common symptoms such as:
- Depression and anxiety
- Being underweight or having a low body mass index (BMI)
- Hypersensitivity to pain, known as central pain sensitization
When to See a Doctor
If you suspect you have symptoms of endometriosis, it's important to consult a healthcare provider. Early diagnosis and treatment can help manage the symptoms and improve quality of life.
- Persistent pelvic pain that disrupts your daily life
- Severe menstrual cramps that do not improve with over-the-counter pain medication
- Difficulty getting pregnant
- Symptoms that resemble other conditions, such as irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID)
Endometriosis can be challenging to manage, but with the right medical care, you can take control of your symptoms and lead a fulfilling life.
Diagnosis of Endometriosis
Initial Consultation and Medical History
Diagnosing endometriosis often starts with a detailed review of your medical history. Your doctor will ask about your symptoms, menstrual cycle, and any difficulties with pregnancy. They will also inquire about pain during periods and other times.
Imaging Tests
To get a clearer picture, your doctor may order imaging tests. Common tests include:
- Ultrasound: Uses sound waves to create images of your organs. A transvaginal ultrasound involves inserting a small wand into the vagina to get a closer look at the reproductive organs.
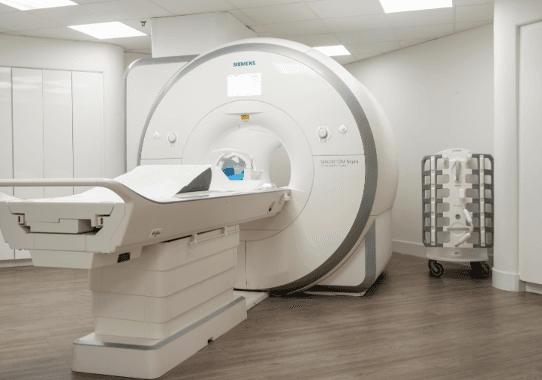
- MRI: Uses magnetic waves to produce detailed images of tissues and organs inside the body. This can help in surgical planning by showing the location and size of endometrial growths.
Laparoscopy for Diagnosis
Sometimes, a definitive diagnosis requires a surgical procedure called laparoscopy. In this minimally invasive surgery, a small incision is made near the belly button. A thin tube with a camera, called a laparoscope, is inserted to examine the abdominal cavity. This allows the surgeon to see and possibly biopsy endometrial tissue.
After the procedure, the doctor will classify the condition based on the location and amount of endometrial tissue. This helps in creating a tailored treatment plan.
Medical Treatments for Endometriosis
Pain Relief Medications
Medications are often the first step in treating endometriosis. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen are commonly used to manage pain. For more severe pain, doctors may prescribe stronger painkillers.
Hormonal Therapies
Hormonal treatments can help control the symptoms of endometriosis by altering hormone levels. These therapies include:
- Oral contraceptives: Pills that contain estrogen and progesterone to regulate hormones.
- Progestins: Medications that stop menstrual periods and the growth of endometrial tissue.
- Gonadotropin-releasing hormone (GnRH) agonists and antagonists: These drugs block the menstrual cycle and lower estrogen levels, causing endometrial tissue to shrink.
- Aromatase inhibitors: Medicines that reduce the amount of estrogen in the body.
Fertility Treatments
For those struggling with infertility due to endometriosis, fertility treatments may be an option. These treatments do not address the symptoms of endometriosis but can help with conception. Options include:
- In vitro fertilization (IVF)
- Fertility medications
It's important to discuss all treatment options with a healthcare provider to find the best plan based on individual needs and goals.
Surgical Options for Endometriosis

Laparoscopic Surgery
Laparoscopic surgery is a common method to treat endometriosis. It involves making small cuts in the abdomen to insert a thin tube with a camera and surgical tools. This allows the surgeon to remove or destroy endometrial tissue. This minimally invasive procedure usually results in shorter recovery times and smaller scars. However, the pain may return over time.
Hysterectomy
A hysterectomy involves removing the uterus and is considered when other treatments have failed. There are two main types:
- Hysterectomy with bilateral salpingo-oophorectomy: This involves removing the uterus, ovaries, and fallopian tubes. It has the highest success rate but requires hormone replacement therapy to manage menopausal symptoms.
- Hysterectomy without bilateral salpingo-oophorectomy: This involves removing the uterus but leaving the ovaries and fallopian tubes intact.
Hysterectomy can relieve pain in 80% to 90% of women, but there is a chance of recurrence.
Post-Surgical Care and Recovery
After surgery, doctors may recommend hormone therapy to help prevent the recurrence of endometriosis. Recovery times vary depending on the type of surgery performed. It's essential to follow your doctor's advice for post-surgical care to ensure the best outcome.
Surgery is often considered when medications fail to relieve endometriosis symptoms. While it can provide significant relief, it's not always a permanent solution, and symptoms may return.
Pain Management Strategies
Medications for Pain Management
Managing pain from endometriosis often involves a combination of medications. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil) and naproxen (Aleve) are commonly used to reduce pain and inflammation. Muscle relaxants such as baclofen and tizanidine can help alleviate muscle cramping and pain. Additionally, antidepressants like amitriptyline and anticonvulsants such as gabapentin are prescribed at lower doses to manage chronic pain.
Physical Therapy and Alternative Treatments
Physical therapy can be a crucial part of managing endometriosis pain. Pelvic floor physical therapy helps relax and strengthen the muscles in the pelvic area, reducing pain. Alternative treatments like acupuncture may also provide relief by targeting specific points on the body to alleviate chronic pain.
Support Groups and Counseling
Living with chronic pain can be emotionally challenging. Support groups offer a space to share experiences and coping strategies. Counseling, including cognitive behavioral therapy (CBT), can help manage the emotional toll of chronic pain and improve overall well-being.
Combining different pain management strategies can significantly improve the quality of life for those suffering from endometriosis.
Living with Endometriosis
Diet and Lifestyle Changes
Making changes to your diet and lifestyle can help manage endometriosis symptoms. Eating a balanced diet rich in fruits, vegetables, and whole grains can reduce inflammation. Regular exercise can also help alleviate pain and improve overall well-being.
Managing Stress and Mental Health
Chronic pain from endometriosis can lead to stress and mental health issues. It's important to find ways to manage stress, such as through meditation, yoga, or talking to a therapist. Support groups can also provide emotional support and practical advice.
Long-term Outlook and Recurrence
Endometriosis is a chronic condition, and symptoms can return even after treatment. Regular follow-ups with your healthcare provider are essential to monitor and manage the condition. While there is no cure, treatments can help improve quality of life.
Conclusion
Endometriosis is a challenging condition that affects many people, causing pain and sometimes fertility issues. While there is no cure, various treatments can help manage the symptoms and improve quality of life. From medications to surgeries, each option has its benefits and potential side effects. It's important to work closely with healthcare providers to find the best treatment plan for your individual needs. Raising awareness and seeking support from groups can also make a significant difference. Remember, early diagnosis and treatment can help manage the condition more effectively.
Frequently Asked Questions
What is endometriosis?
Endometriosis is a condition where tissue similar to the lining inside the uterus grows outside of it. This can cause pain, especially during periods, and may lead to fertility problems.
What are common symptoms of endometriosis?
Common symptoms include pelvic pain, heavy periods, pain during intercourse, and pain with bowel movements or urination. Some people may also experience fatigue, diarrhea, constipation, and bloating.
How is endometriosis diagnosed?
Doctors may start with a pelvic exam, ultrasound, or MRI to look for signs of endometriosis. A definitive diagnosis often requires a laparoscopy, a minor surgery where a camera is used to see inside the abdomen.
What treatments are available for endometriosis?
Treatment options include pain relief medications, hormonal therapies, and surgery to remove endometriosis tissue. The choice of treatment depends on the severity of symptoms and whether the patient wants to become pregnant.
Can endometriosis affect fertility?
Yes, endometriosis can make it harder to get pregnant. However, treatments are available that can help improve fertility, including medications and surgical procedures.
Is there a cure for endometriosis?
There is no cure for endometriosis, but treatments can help manage symptoms and improve quality of life. Options include medications, hormone therapy, and surgery.